It has been six months since my Clinical Practice I (CP1), and I am returning to CP2. These are the timelines:
| Week | Posting |
|---|---|
| 1 | Mental Health – IMH |
| 2 | Primary Healthcare Services – Polyclinic |
| 3 – 4 | Acute Hospital – Surgical |
| 5 – 9 | Acute Hospital – Medical |
Compared to CP1, I have a week less and 3 Public Holidays (Labour Day, Labour Day, and Vesak Day). This means I only have four training days at the Polyclinic and eight training days in the surgical ward. One of the days is taken up by the Next Generation Electronic Record (NGEMR) training on the Tuesday of Week 3, where we are trained to become better navigators through the EPIC system, which I will use during my attachment. The posting varies and may not be in the same sequence. As there are over 300 nursing students per cohort, segregation is required. Some might start with their Primary Healthcare Services, Surgical or Medical posting. Before the posting, we must complete the same Data Governance & Protection, IT Security Quiz and Letter of Undertaking as we did in our CP1. An e-learning account has also been created for us to access these resources, and we received a clinical placement information sheet on which ward we are going to and who our clinical instructors (CI) are. In the surgical ward, we have the same CI throughout the two weeks and in the medical ward, due to last-minute changes, we have two same CIs for Week 3 and Week 4 to 5, while Week 1-2 is a trainee CI from another ward. We were also told we have an additional new trainee CI in Week 4, so we were fortunate.
In this CP2, 75% of the 26 Year 2 skills must be competent, including all Year 1 revision skills. To achieve 75%, 19 skills are required for male students and 20 for female students, as there is a urinary indwelling/intermittent catheterisation for a female patient that male students are not allowed to perform.
The required levels of competency are I (Independent), S (Supervised), and A (Assisted).
Skills marked with an asterisk * are critical skills that can only be signed by an Assistant Nurse Clinician (ANC) or above, CI, or my school Clinical Facilitator (CF). They are also mandatory to complete.
The other skills can only be signed by an Enrolled Nurse (EN) and above who has graduated over two years.
Initial practice means that it is the first time the student performs the skill and can perform at least 50% competently.
Completed skill satisfactorily requires the student to perform at least 80% competently on their subsequent attempt.
Confirmation of ability to perform skill is to be acknowledged by the student after both initial practice and completed skill satisfactorily is signed.
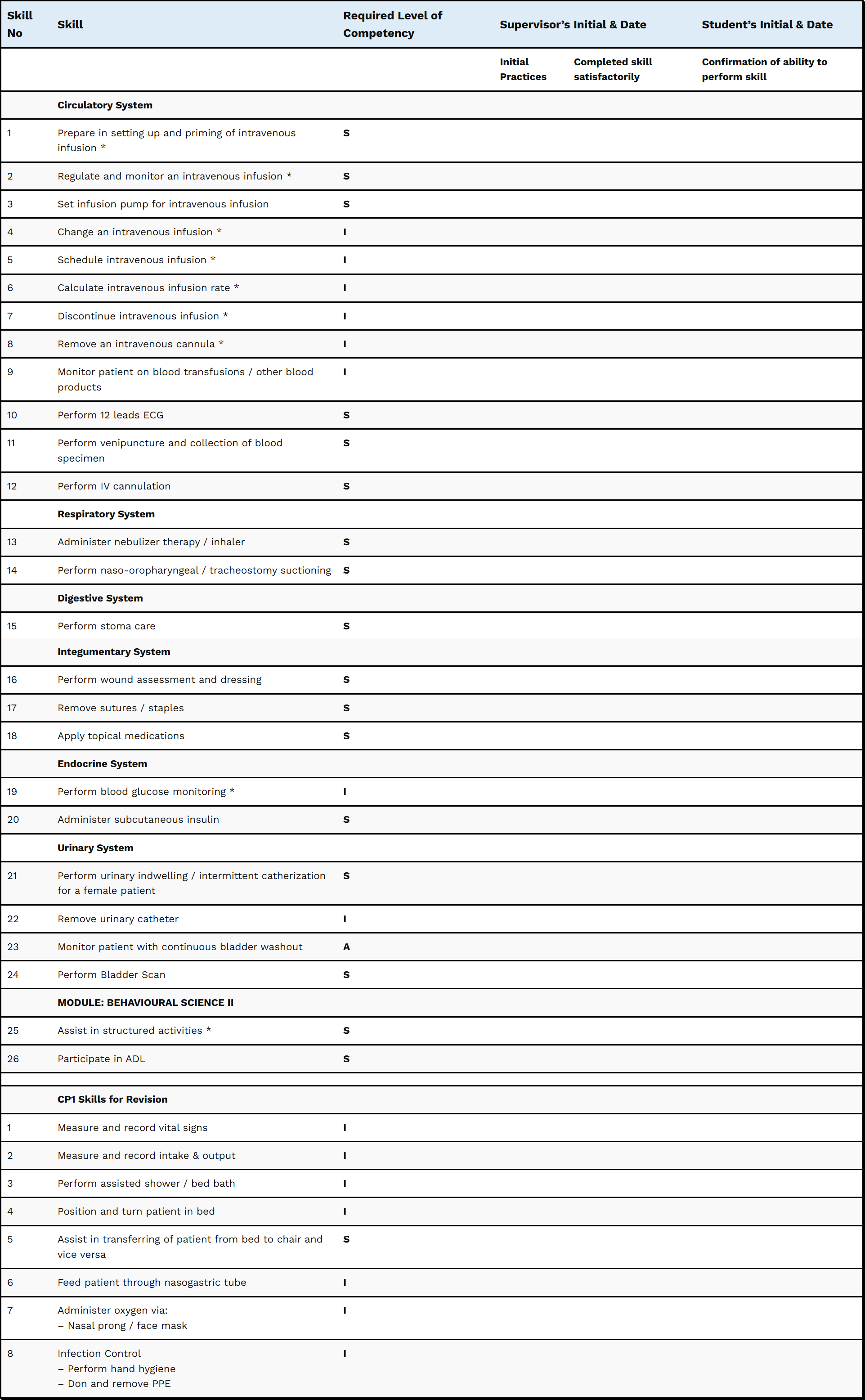
Initial Practice and Completed skill satisfaction must be at least three working days apart (these exclude Saturday, Sunday, and Public Holidays).
Depending on the ward you are attached to, you might be unable to perform the skills. For instance, if you are attached to a ward that specialises in renal, don’t expect to be able to perform IV skills. However, do not worry, as your CI or CF will be able to simulate it so that you can get your skills signed. As much as possible, approach your CI first, and if your CI isn’t available, you may approach your CF, as the school is paying for the CI service (yes, this is something that not many people know about). Skill No. 23 Monitor patient with continuous bladder washout and 15 Perform stoma care is a rare skill, so it is okay if you do not have the opportunity. In my case, I am fortunate to be in a Fast Medicine ward, which means I have more opportunities to complete the skills. Skill No. 6 Feed patient through nasogastric tube came in the last weeks of my medical posting, and I only managed to see one patient with tracheostomy suctioning and the other with stoma care. Always take the opportunity to perform the skills, and if you are waiting three working days apart, you may want to give the chance to your other group of students to perform their skills if they have not done so yet. And please, even if you have completed the skills satisfactorily, continue to practice them and do not do it only to get the skills signed.
CF and CI have the right to reassess your skills at any time. Remember, you might not always be fortunate enough to get the same CI in the future, and if you are unlucky enough to get someone who wants a probation standard or higher, then I wish you all the best. For your information, ever since CP1, the final batch of Nitec students, Pre-enrollment Clinical Practice (PECP) and the current CP2. There have been some changes, and your performance is being e-graded by your CIs. Even though your performance is good in the view of your CIs, your CF can deduct your grade at any point. Having good overall feedback doesn’t necessarily mean you have a high score. You will be graded based on:
| # | Professional Attributes | Skills Proficiency |
|---|---|---|
| 1 | Professional image | Demonstration of concern for patient |
| 2 | Punctuality | Assessment |
| 3 | Acceptance of guidance | Planning |
| 4 | Participation in patient care | Implementation |
| 5 | Communication | Evaluation |
| 6 | Teamwork | Health Education |
| 7 | Initiative | Use of equipment and supplies |
| 8 | Time Management | Quality of Performance |
| 9 | Ability to problem solve | Performance Rating – Exemplary / Proficient / Developing / Emerging / Incompetent |
| 10 | Integrity, responsibility and accountability | *Every component is graded individually. In order to Pass, you must get Developing and above. |
As usual, the school gives an allowance of $35 per working day from the ministry, which applies to all students. On the final week Thursday of my medical posting, I took a sick leave (Medical Certificate); this means that I have to do the make-up on the following week, Monday, as Saturday is a Public Holiday (Hari Raya Haji). No make-ups are to be done on Sundays and Public Holidays, and no allowance will be given.
Mental Health – IMH
Date: 7-11 April 2025 (Week 1)
Shift Hours: 0800-1500 (AM), 1300-2100 (PM), 0745-1630 (Orientation)
Day 1 (Orientation)
I reported to the Lecture Hall, and before I went in, I had to find my name on the nominal roll to know which ward we would be going to and sign my attendance, as we were being grouped into different wards. As this is a special posting, I managed to see some of my classmates and other groups of students who are not from the same hospital. These include students in the 2-year Higher Nitec in Nursing (April intake), as they are doing their CP2 at the same time as us. The only difference is that they have completed their Behavioural Science module, which we will do after our CP2.
Once I was seated in the hall, the whole day was mainly orientation, administrative matters, rules and regulations, and sharing by the CIs. We were introduced to multiple CIs, and they had to manage various groups of students going to different wards. Unlike the medical and surgical postings, there are individual CIs per ward. We were given a short break in between, and after our long lunch break, we went to the museum. Shortly after, we went on tour to the respective wards to which we were assigned. My group members and I went to the acute general psychiatry ward. It was mind-blowing as this is not an experience we see daily, and it affects my emotions partially. After a short tour of the ward, we went to the educational office before the end of our day to discuss what we observed with our CI, an ANC. Our findings were:
1. Upon opening the door with an access card, the door has to be closed for the other door to be opened. This is to prevent patients from absconding.
2. Staff do not wear lanyards in the ward to show their staff pass, and they are using retractable clips. This is to prevent strangulation.
3. Staff carry an emergency panic button. This can be used in the event of a crisis.
4. The chairs are cumbersome. This is to prevent patients from throwing at one another.
5. The water will only flow with motion and no soap, to prevent the patient from drinking. There are no hand rub bottles, either. Every staff member, including students, is given a small retractable hand rub bottle.
6. The fire extinguisher and television are being locked in a cabinet.
7. The bed is not like your usual hospital bed; there are no wires to prevent strangulation.
8. There is no headboard; patients can roam wherever they want.
9. There is an isolated room for patients who require special care.
10. An Auxiliary Enforcement Police Officer (AEPO) guards the ward and may be activated in a crisis.
Day 2-5
After a day had passed, my emotions were better. The day-to-day activities were quite similar in my Senior Citizen Care Centre (SCCC) posting in CP1, where we had to interact with clients in the senior care centre and dementia care centre, except that the cases were mainly Schizophrenia and Intellectual Disability (ID). I continued to observe the patient’s daily activities, talk to them, and play carrom with them. They are experts in it and win most of the time.

One requirement for this special posting is to conduct a simple and engaging structured activity by Day 4. My group members and I created a structured activity. Thanks to our CI, who provided an Instagram profile from which we could get our ideas.
The game has two difficulty levels. The easiest version involves throwing the crumpled paper into the box with the highest points. A more challenging version involves shooting the crumpled paper using a plastic cup, and the balloon will act as a slingshot. It sounds easy, but it isn’t as easy as it seems. We even had difficulty scoring points.
We crafted the box using the InstaChef box and brought our own paper and writing materials. Our CI also offered us the materials and cardboard boxes if required.
One of my group members talked to a patient regarding our Biological Science II (BIO2) module, which we learnt in school. It turns out that the patient could answer all the questions correctly. The patient is better than us, and please do not underestimate them. Thanks to the health education provided to the patients, they even know why they are on a specific medication and the importance of taking it. They are there because of their condition.
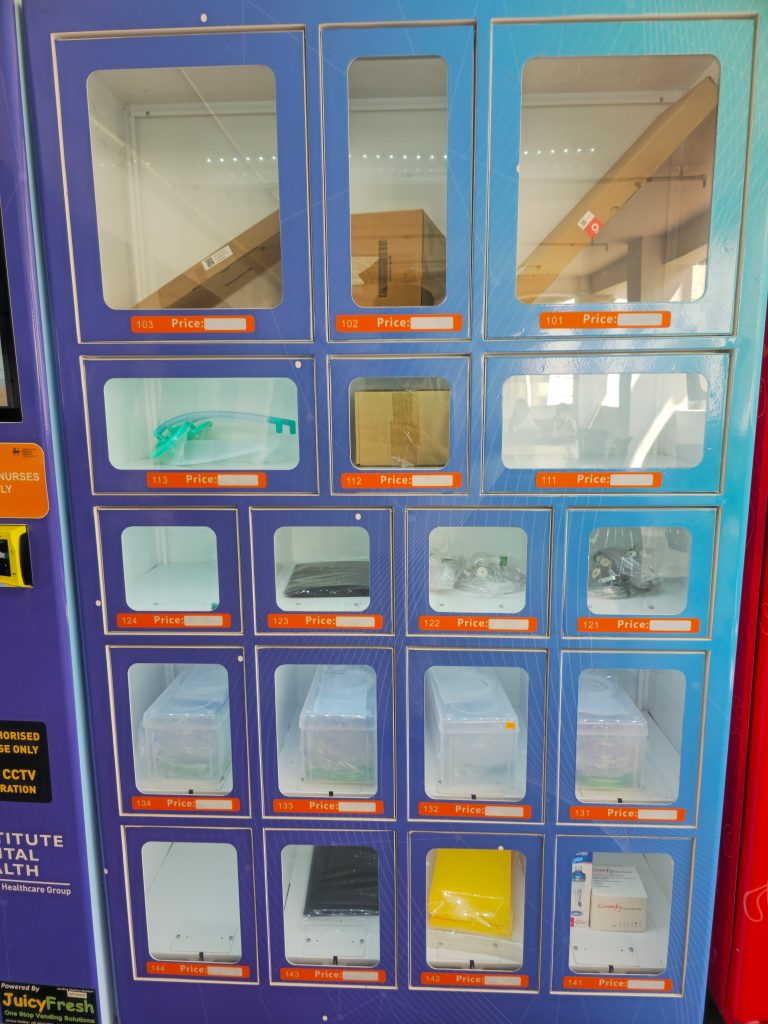
Parking is free if you are driving. This is to encourage visitors, and I recommend you bring your food, especially if you are doing the PM shift. The only options are 7-Eleven, InstaChef, or a sandwich machine. There is also a GrabFood Smart Food Locker, should you want to order GrabFood. The vending machine might be a good option if you are thirsty because the drinks are relatively cheap.
There is also a cool vending machine where staff can buy medical supplies for their wards if they lack them.

Throughout the posting, I was pretty fortunate as there wasn’t a crisis in my ward compared to the others. Mental Health is one of the specialities that I might be interested in. As such, I have signed up as a volunteer and hope to explore this field more before making a final decision.
Polyclinic
Date: 14-17 April 2025 (Week 2)
Shift Hours: 0800-1600 (Office Hours), 0750-1600 (Orientation)
Day 1 (Orientation)
We were told to report to Level 3 of the waiting area, and shortly after our CI arrived, an ANC arrived. We signed our attendance, and we were brought to the meeting room. In the meeting room, we were briefed on the institution and the services offered. It turns out that there is also a satellite mental health clinic on the same level.
By the end of this special posting, we will need to complete the Primary Healthcare Services worksheet. The information can be sourced through the individual service station that we are assigned to or the organisation’s website. On the first day, I was assigned to the Wound Dressing service station and observed how a simple wound dressing and Suture-To-Off (STO) were done.
Day 2-4
On Day 2 in the morning, I was still attached to the wound dressing station and managed to assist with simple wound dressing and Multi-Drug Resistant Organisms (MRDO) wound dressing. After my lunch break and throughout the rest of the day, I managed to explore the Women & Child Health Services, Immunisation/Vaccination Programme, Diabetic Screening (Foot screening, Diabetic Retinal Photography), Health Promotion/Education, and Directly Observed Therapy (DOT) for Tuberculosis clients. Most nurses I came across hold the Senior Staff Nurse (SSN) position. I also encountered an experienced Care Coordinator who shared her experiences with me.
Our CI has also allowed us to examine how a Medical Registrar removes earwax for one of the patients through ear syringing.

The week ended fast, as Labour Day falls on Friday. Overall, it was a good learning experience, and I explored all the service stations (except for a Pap smear and mammogram, as I am a male student).
Surgical
Date: 23 April – 2 May 2025 (Week 3-4)
Shift Hours: 0800-1600 (AM), 1300-2100 (PM), 0800-1600 (First Day), 0800-1700 (NGEMR Training)
Day 1 (Orientation)
I reported to the same ward, and there wasn’t much orientation. However, there were some slight updates, and we were being briefed. One of the updates was having to do an e-attendance when signing in and out of duty. I was attached to the same CI as back in CP1, and shortly after the briefing, we were assigned to the cubicle where we would commence our duties. Although it is a surgical ward, only 10 beds are for surgical patients. The rest are still under Fast Medicine, which has been six months since CP1. I am trying to recover the memory of things I have learnt, and it gets better towards the end of the day than in the morning.
Day 2 (NGEMR Training)
When I return to the hospital, new blocks are constantly being built. When I wasn’t a student yet, there was only a hospital. When I came for my CP1, a rehabilitation block had been built, and when I attended the NGEMR training, it was in another new block. Some students from another hospital also have to come to my hospital for their training. The training used to be two days, but they have compressed it into one day. However, the duration is long, so it is pretty hectic. But at the end of the day, we became better navigators of the EPIC system, and one of the jokes shared by the trainer is. Only nurses have brains. The brain is a feature that allows nurses to see their to-do lists and overdue tasks, such as assessments to be done, vital signs, and medications to be administered.
For the rest of the days, I continued to find skills I could perform, as these are the criteria for passing CP2. There wasn’t any issue with the skill. Although it is a surgical ward, it is still rare to see cases of continuous bladder washout. Our CF also gave us a case study worksheet, where we had to perform our case study presentation in the final week; although it is not a requirement of CP2, she has the best interests at heart.
I received a gift and a note from one of the SNs and felt touched.

After the final week, things improved from the first day, and I felt more confident when performing procedures. I met some Year 3 National University of Singapore (NUS) nursing students attached to the ward. Some are graduating after their current Final Year Transition-to-Professional Practice (TTP) posting, while the Honours have another year to go. I also learned that we are the first institution to be able to perform IV cannulation as a student. An Enrolled Nurse (EN) might be given more roles once they achieve a particular competency.
Medical
Date: 5 May – 6 June 2025 (Week 5-9), Make-up (9 Jun)
Shift Hours: 0800-1600 (PM), 1300-2100, 0800-1600 (First Day)
On my first day, we were attached to a new trainee CI, an SSN from an isolation ward, and he will be with us for two weeks. An interesting thing about him is that he always asks why for a particular question and will try to elaborate more. There is no right or wrong, and he will try to elaborate if it’s a wrong answer.
In the second week, there was an ice cream booth right outside the cafeteria, and we were told to collect the ice cream in the afternoon; shortly after we collected, we went to a room in a new block that we had shared with the Senior Nurse Educator (SNE) and NE on what we had learnt so far, and they gave us advice as well.
We had the same CI in the third week, and she helped us complete the skills we still needed.
In the fourth week, we had another CI and a trainee CI from the same ward. They are also working on helping us achieve our skills. In the afternoon, we were brought to the auditorium, where there was a hackathon-sharing session. Although it was only an hour, I saw the healthcare system’s innovations and future. We also had to perform a case study presentation. It was the most hectic week across my posting, as the cases had been smooth over the past few weeks, and many activities of daily living (ADLs) needed to be done this week. Things are unpredictable and can happen anytime. Rare skills like NGT feeding and nasopharyngeal/tracheostomy suctioning start to pop up. However, I have no regrets as this is a good opportunity to learn the most. There was a three-month exchange programme between the Fast Medicine and Rehabilitation wards, where some nurses were involved. Through these, I managed to see even more individual skills, and those beneficial ones would improve my learning and help me to be a better future nurse. As I always believed, there is always room for improvement.
As the final week came, I continued to practice the things I was being taught and applied them. On my replacement day, it felt different as I was the only student in the ward. The nurses were like, “Why are you still here?” I managed to see a Work-Study Diploma (WSDip) nurse back to his ward as I hadn’t seen him since my last posting, and my PCB lecturer came down too, as she is also teaching him.
CP3 will be two weeks in January 2026, and the remaining weeks will be on campus. The April intake will be doing their PECP, and for the January intake, the PECP will be from October to December.
It will be another long-term, and I have nearly achieved the 50% milestone. Another 50% to go, and I will be graduating 🙂