I am back for my Clinical Practice I (CP1) after a one-month term break on 8 July 2024. It was a long break, and I was excited because I was more practical. After six months of school, I can now apply the skills I have learned to an actual human rather than a dummy. These are the timelines:
| Week | Posting |
|---|---|
| 1 – 2 | ILTC – Nursing Home (NH) |
| 3 | ILTC – Senior Citizen Care Centre (SCCC) |
| 4 – 5 | Acute Hospital – Surgical |
| 6 – 10 | Acute Hospital – Medical |
During our term break and about one week before my CP1 started, I had to complete e-learning for the hospital attachment. It consists of an overview of the hospital, Patient Safety: 6 IPSG, PDPA & IT Security, Incident Reporting System, Fire safety & Emergency information, and Infection Control and management.
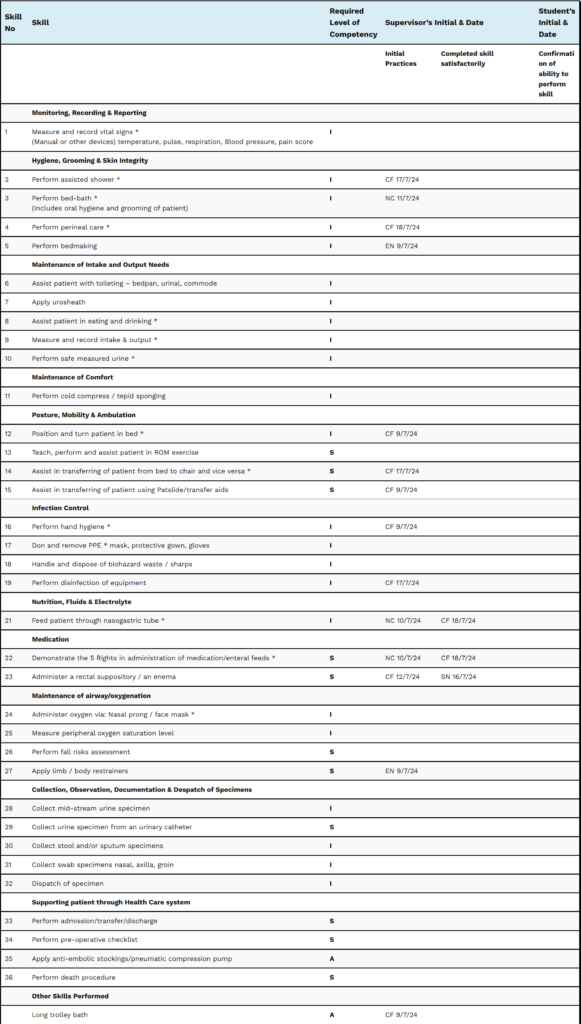
In this CP1, 75% of 36 skills must be competent.
The required levels of competency are I (Independent), S (Supervised), and A (Assisted).
Skills marked with an asterisk * are critical skills that can only be signed by an Assistant Nurse Clinician (ANC) or above, Clinical Instructor (CI), or my school Clinical Facilitator (CF). They are also mandatory to complete.
The other skills can only be signed by an Enrolled Nurse (EN) and above who has graduated over two years.
Initial practice means that it is the first time the student performs the skill and can perform at least 50% competently.
Completed skill satisfactorily requires the student to perform at least 80% competently on their subsequent attempt.
Confirmation of ability to perform skill is to be acknowledged by the student after both initial practice and completed skill satisfactorily is signed.
The school gives an allowance of $35 per working day from the ministry and applies to all students.
NH
Date: 8-21 July 2024 (Week 1 & 2)
Shift Hours: 0730-1530 (AM), 1230-2030 (PM), 0800-1600 (Orientation)
Day 1 (Orientation)
It brings back some memories of when I went for clinical attachment as a therapy support trainee almost a year ago (August 2023). It’s the same organisation, just a different location. I reported to the NH at 0745 hours. There were a total of eight nursing students from our school. I am the only male and oldest in the group. It was an orientation day, and we started by being briefed by the CI, a Nurse Clinician (NC) from the NH. My CF was present, and we received the assignment guidelines for our SCCC posting.
After the briefing, two students were attached to each level (accommodation) and on my level, I was connected to a Senior Nursing Aide (SNA) to show us around. For the rest of the day, until 1540 hours, I observed how the NH functions and was given a one-hour break. The organisation that we are in has a flexible break time. You can either clear your break time in one shot or split them.
Closer to the end of the day, a resident was curious about me and wanted to know more. I interacted with him for quite a while, and he gave me three riddles to solve. Afterwards, it was tea time, and I managed to distribute the drinks and assist in feeding a packet of biscuits to a visually impaired resident.
At 1540 hours, I signed out and went to a room. Our school Section Head (SH) then rebriefed us about CP1 matters.
Day 2 (AM)
I was attached to an EN. I observed the procedure of bed making, oral swabs, and Nasogastric Tube (NGT) feeding. My CF passed by, and I managed to perform a long trolley bath on a resident with a Nursing Aide (NA). My EN also showed me how to apply body vest restraint and the principles. I have to thank the nursing staff for taking good care of us; it is not easy for them, and I told myself that I am not only here to learn and get my skills signed, but I would like to help them as much as possible to lower their load. There are 57 residents on my level, only 1-2 Staff Nurses (SN), 1 or 0 EN, and the rest are NA/SNA throughout the day. I find that the knowledge of the NA/SNA is better than that of most local locum EN/RN I have ever encountered. Shouldn’t local nurses be more caring?
Day 3 (AM)
I performed an oral swab before feeding the two residents via NGT, and there is room for improvement. It was so coincidental that my CF observed me in the morning and CI in the afternoon. The best part is that the aspiration amount was just droplets; pH was 6.5 for the first resident and 6.0 for the second resident, as I was expecting to get a higher aspiration amount. This experience immediately led me to learn something new. After finishing the procedure for the first resident, I managed to don my Personal Protective Equipment (PPE) and enter an isolation room to perform a Percutaneous Endoscopic Gastrostomy (PEG) tube feeding for a resident with scabies. After my shift had ended, I got to see how the SN did the wound dressing.
Day 4 (PM)
It feels like I am on Day 3, except it’s my first afternoon shift. At 1430 hours, our nursing students visited a meeting room to meet the CI. We learned about EatSafe, signed our logbook, and had a Q&A session. During dinner for the residents, I learned to prepare the meals as delivered by the cookhouse by scooping manually for each resident according to their International Dysphagia Diet Standardisation Initiative (IDDSI) framework level and adding the required amount of thickener to ensure consistency for the food and fluid. I managed to perform more oral feeding on residents who needed assistance. It was so satisfying, and started to bring back my memories while working as a Healthcare Assistant (HCA) in a Transitional Care Facility (TCF) back then. After dinner, I managed to feed medications and milk supplements to NGT and PEG tube residents under close supervision. It shows me the importance of performing five rights before administering medications. I am even more confident now in my NGT and PEG tube feeding.
Day 5 (PM)
It is just one more day towards the weekend, my rest day. I managed to administer a rectal suppository, as I always thought that it was a challenging procedure. Until I tried, it didn’t seem as hard as it is. Throughout the week, I am already used to the routine. The more I practice, the more confident I become, and interestingly, everyone has their style of doing things.
Day 8-9 (PM)
Usually, after 1700 hours, there is nothing much, and I would prefer the AM shift as there are more things to do, and time flies faster. I communicated more with the SN on general topics, such as infection control, better ways to administer rectal suppositories, and administering an inhaler with a spacer.
Day 10 (AM)
I am finally back on the AM shift after four consecutive PM shifts. Our CF has been reminding us to complete the critical skills and have them signed by her or the CI. I performed multiple skills at once while bringing the resident with an IDC (indwelling urinary catheter) for assisted showering through the commode.I think that attitude is essential. I have taught new joiners before, and it isn't easy to teach someone because it will take additional time on top of your original job scope. As a student nurse, I shouldn't have the mindset that I am ONLY there to get the skills signed. Instead, I should be learning and helping to lower the workload for the staff as much as possible. It applies to studying, too. Would you study to get good grades and throw everything away after graduation, or would you like to have the knowledge even after decades? "Time will tell; patience is the key to success."
Back to the topic, in the afternoon. I managed to instil eye drops for some of the residents. Although it seems to be bare, it is pretty interesting, too.
I have observed why specific procedures have different ways of being done, as costs and budgets play a part. I am thankful for my years of working experience as it allows me to see things in a bigger picture.
Day 12 (Last Day, AM)
Almost x2/52 (two weeks) have passed quickly; it will be my last day at the NH. My group of students would be on the AM shift, and those who have to do replacement would have to do it on Saturday. My CF, my buddy, and I spent some time doing the thank you cards, and a few days back, my buddy suggested preparing and giving a gift to over 30 staff based on the name list she had obtained. Look at the idea that she came up with:

After the afternoon roll call, we started giving out the gifts and took a group photo with the staff.

Not all the staff are in the photo; some are busy or off day or working PM or ND (night duty).
We appreciate the staff showing us Tender Loving Care (TLC) during our ILTC (Intermediate And Long-Term Care) NH CP1 attachment and hope we managed to help the staff in specific ways.
We managed to practice most of the skills and observed additional skills, which is beneficial and will help us in our nursing journey in the coming years or even decades. We also appreciate the SN, EN, and NA for going the extra mile. I was pretty sad as I had seen things throughout my years working in healthcare, and I knew this was a rare and golden opportunity for a learning experience. I wonder when the same opportunity will arise.
Although I only spent time with the residents for around x2/52, many have their own stories, and most are sad. Sometimes, they are in a low mood; we should be emphatic with them as given a choice: would you rather stay at your own home or an NH? I was also quite touched that one of the residents wanted to give me a tremendous gift. However, I had to tell him I appreciated it but couldn’t accept it. As HCWs, we must remain professional and abide by the four ethics that I used to learn as a therapy support trainee. Respect autonomy and uphold justice, beneficence, and non-maleficence.
After the roll call, my buddy and I proceeded to the office to pass our thank you cards and gifts to the management. I also went to a meeting room where we had a 1:1 session with the CI and our CF to check my clinical logbook, which has been with the CI for the past two days. Inside the logbook, the CI and CF signed any outstanding skills I have performed, and the CI gave overall feedback on my performance at the NH. After acknowledging my feedback, I had to submit a form to provide feedback on them during my x2/52 at the NH.

Before our shift ended, I learned to auscultate a resident using a stethoscope to check whether the NGT was in the correct placement as a last resort. My buddy and I interacted more with the staff and residents. The Nurse Managers (NMs) invited us to their organisation, Nurses’ Day 2024. On Day 11 (Thursday), there was a durian activity, and they asked us to have durians with the residents and staff before we went back home. I didn’t join as I am currently on a ketogenic diet, but some students from my group joined.
The same NH organisation I work for always plans daily activities for residents. For instance, when I went for my clinical attachment last year, there were snow-skin moon cake making, cat therapy, baking, sewing, gardening, karaoke, spiritual activities, picnics, and many more. They also have a birthday cake for residents born in the birthday month.
What I like about this organisation is that they want the residents to participate as much as possible when doing their ADLs (activities of daily living) to promote independence. The residents will be transferred to the day space during tea and meal times, preventing them from staying in bed for prolonged durations, leading to pressure sores.
Also, I recall a reward system in which the residents received a voucher when participating in activities, which they could use to exchange nostalgic daily essential items.

In this ILTC NH posting, I have performed 15 skills (nine critical, five ordinary, and one additional). I only booked once for NGT feeding. Most other skills are signed when the CI or CF pass by and observe me.
Critical Skills: Perform assisted shower, Perform bed-bath (Includes oral hygiene and grooming of patient, Perform perineal care, Perform safe measured urine, Position and turn patient in bed, Assist in transferring of patient from bed to chair and vice versa, Perform hand hygiene, Feed patient through nasogastric tube, and Demonstrate the 5 Rights in administration of medication/enteral feeds.
Ordinary Skills: Perform bed making, Assist in transferring of patient using Patslide/transfer aids, Perform disinfection of equipment, Administer a rectal suppository / an enema, and Apply limb / body restrainers.
Additional Skill: Long trolley bath
There were some skills that my CF had forgotten to sign on certain days, but it didn’t matter much to me as I knew that it was a generally available skill and that I would get to perform again. There were also many skills that I have performed but have yet to be signed due to the limited EN or SN, as I was with the NA most of the time. So, always plan and book the critical skills you want to perform with your ANC and above, CI or CF. And EN and above for ordinary skills. To be considerate, book multiple skills at once rather than individually and in advance.
For example, as you can see, on 9 July 2024 (Day 2), I was going to perform an additional skill (long trolley bath). But to do that, I had to Perform and turn patient in bed, Assist in transferring of patient using Patslide/transfer aids, and, after the bath, perform hand hygiene. Got four skills signed at once. You would want to perform skills only available to the specific place you are being posted first rather than skills generally available everywhere. An example would be Feed patient through nasogastric tube, as you might not have a chance to do it when posted to an acute hospital, depending on the ward that you are in.
SCCC
Date: 22-28 July 2024 (Week 3)
Time: 0800-1600 hours
I am back at my SCCC posting after the weekend. I didn’t have much rest as I had a befriending CCA on Saturday, and I had been working on the pamphlet, a group project where I had to find out the information:
Overview of the Senior Citizen Centre (Purpose/objectives of the centre, Services available, Operating hours, Maximum capacity of the centre)
Clients’ Profile (Age group, Medical conditions, Frequency of visit to the centre per week, Length of stay per visit)
Familiarisation with the Centre (Layout of the centre, Purpose of each area of the centre, List of equipment and purpose of each equipment, Timetable of activities)
Healthcare Team (Members of the healthcare team, Roles and responsibilities of each member)
Day 1
My group of students, four of us, is attached to a Senior Day Care Centre at level 1 of an HDB (Housing & Development Board), and as usual, we are to report at least 10 minutes earlier. On the day, my CF was present and had to travel to multiple sites as another group of students was at another location.
I saw the Centre Supervisor while waiting for the Community Nurse, a registered nurse (RN), to arrive. Our CF goes through the things that we need to do during our posting, which includes having our assisting ROM (range of motion) skills signed, the pamphlet group project and an individual reflection journal in which I have to interact with a client (senior citizen) to find out:
1. Reasons for the use of services as stated
2. Benefits of the services
3. Learning points that I have learned
And the personal reflection of my SCC posting.
I would also have to coordinate with the Centre Supervisor to organise a structured activity, and our CF must be present on the actual day to see us perform.
When the Community Nurse arrived, we were introduced and orientated on the centre’s layout, the timetable of activities, the activity area, and the nurse room. They have two centres, and she has to manage both opposite the block.
After the orientation, we split into groups of two. One of the groups will go to the other block, and the other group will remain in the same block. It will switch daily, and the block we are in is clients that require dementia care, while the other block is mostly maintenance care. Most of them also have the risk of falls. We have to inform the staff if a client stood and to ensure that they did not abscond as they were supposed to be in the centre until their next-of-kin (NOK) picked them up or transported them back to the home by the escort staff; the concept is similar to a childcare centre.
In the morning, all the clients are seated in the activity area. The client’s helper and staff were also present. The staff played relaxing background music, and either a premade or a virtual exercise was conducted virtually by the SCCC’s organisation headquarters.
The exercise seems easy, but it can be tiring after engaging in it. This shows the importance of working different parts of the body.
After the exercise, I observed how the staff conducted basic occupational therapy activities like colouring, clay making, and fishing; a string tied to a cut soccer cone, and when the staff prompted colour, the client had to throw and make sure that the crumpled paper ball is inside the soccer cone with the right colour. During lunch, we helped serve the clients’ meals, and we went for our break shortly after.
When we ended our break, four students went to the other block to see how the NAs conducted simple physiotherapy activities with the clients using resistance bands, and we participated. It was tea time shortly after, and the staff served them all with a barley dessert. Yes, they are not on a consistency restriction. When they finished their tea time, we provided health education to two clients on hand hygiene and the safety features of a rollator frame and wheelchair. We also practised taking parameters (vital signs) on the Community Nurse and were told about their organisation’s Blood Pressure (BP) baseline.
We then returned to my original block, where we had one hour to discuss group work before we ended work.
Day 2
It is kind of a routine, similar to NH, where most daily activities are the same. The chance to interview one of the clients, Mdm C, in the afternoon for my individual reflection journal was fascinating and significant. These real-life experiences are rare and offer a wealth of knowledge. As I missed out on the earlier part on day 1, I captured the complete activities on day 2.
Mdm C has been in the centre for over a year and lives nearby. She has to wait for transport to pick her up from her home and take her to the centre, and from the centre when she goes back home. She is staying in the centre because her NOK is working. Mdm C is happy in the centre because she can interact with other senior citizens, knowing the importance of exercise, which helps her stay more vital, and meals provided. However, she mentioned that the food tastes average and that she likes singing as there is nothing much to do at her age.
Through my interview with Mdm C, I found that knowing additional language is essential. It allows me to interact and understand more people, an extra motivation to persist in my studies, the importance of staying healthy, and doing things while I still can. It is essential always to remain honest to gain a client’s trust so that there is a higher chance that a client will listen to you when you give them instructions to follow. Everyone does their job and helps one another, which is critical for good teamwork. The centre supervisor, who covered transporting clients’ duties, helped distribute the workload and prevent burnout, which can lead to more issues from happening. Safety is the number one priority, and the staff is always there to monitor the clients should they stand to prevent falls, which could lead to further complications as they are more vulnerable to injuries. The best possible care can be provided to clients by following the proper protocols to reduce or prevent injuries. Always ask for assistance if needed.
The two most common rehabilitation exercises I have seen in the centre are moving the upper and lower limbs through an active range of motion when a video is projected and using a resistance band during a simple physiotherapy exercise, which can reduce the risk of contractures. As for occupational therapy activities, they would involve colouring on a piece of paper and mixing and matching puzzles, which improves fine motor skills.
For the group structured activity, I have to inform my CF what I plan to do by day two and have decided to go with the idea of making a National Day paper flag for the senior citizens. As my group members had no other opinions, National Day is approaching. It is an activity I did at my CCA last Saturday, and it went smoothly. The activity is supposed to take place on Thursday. However, my CF isn’t free, so she asked whether we could do it on Wednesday instead, and we proceeded. After my shift ended, I went to buy the necessary items to prepare.
Day 3
We prepared the items before the group structured activity started at 1045 hours, and the activity had to last around 20 to 30 minutes, as the occupational therapist (OT) recommended. It turns out that I have to do the talking. Thankfully, there were staff to assist, and during the activity, we assisted the clients in making the flag and playing nostalgic National Day songs. The activity went as planned, and the timing was excellent: 30 minutes. After the activity, I served the meals and played relaxing background music, and it felt like a fine dining restaurant.
Day 4
It is the last day to submit the individual reflection journal and group pamphlet, which I must submit by 1200 hours.
(click to view the pamphlet)
There was a bingo activity in which staff announced a number, and the clients with a whole horizontal or vertical number could win prizes. The clients on my left and right won the first and second prizes. Those who didn’t win received tissue paper for participating.
Day 5
The staff shared a fascinating insight with the clients in an online Chinese-language news article about a man who went to Johor Bahru Mall for a massage and signed a package for treatment. Still, after cupping, his back was full of blisters, and he spent 800 yuan on treatment.
I had to ensure that my assisted patient in ROM skills was competent and signed. My CF gave me overall feedback during my posting here, which I must acknowledge.
I will miss the staff: community nurse, centre supervisor, community care associate (CCA), care associate (CA), nursing aide (NA), and driver who guided us through the journey and the opportunities to interact with the clients’.
Surgical
Date: 29 July 2024 – 11 August 2024 (Week 4-5)
Shift: 0800-1600 (AM), 1300-2100 (PM), 0800-1600 (Orientation)
Day 1 (Orientation)
Together with my CF and group members, we reported to the training room at 0745 hours for orientation. The ANC, our ward CI and, the rest of the SSNs (Senior Staff Nurses), trainees from other wards who will also be our CIs are in the room. A box, which is a bag, was given. The organisation’s Chief Nurse (CN) gave a welcome speech, 6 IPSG by a Nurse Educator (NE), sponsorship matters by human resources, Fulmer SPICES and case studies by SNs. Finally, a debriefing by the ADoN (Assistant Director of Nursing) and we received two reflection books published by the organisation.
Yay, my CF has assigned the other student to become a Student Leader. After the orientation, we went to our surgical ward to put on our belongings before we headed for lunch at the cafeteria. Once we were back, we headed to log in to the computer with the credentials given to us. Then we went to the organisation’s Nurses’ Day 2024 activities at the Auditorium, available until 1 August 2024.

The place looks big initially, but if you know the shortcuts, it isn’t as big as it seems. The atmosphere is cosy, and the ward looks like a cafe. Unlike NH, I saw staff from other multidisciplinary teams (MDT).
Day 2 (PM)
I took a parameter (vital signs) on a patient (pt) using the Carescape V100 Dinamap Vital Signs Monitor integrated with a touch screen above. It was different from the past BP machines that I had used. The touch screen allows automatic retrieval of vital signs from the Dinamap and information to be entered such as route of temperature (T), respiration rate (RR) with clock timer, oxygen saturation (SpO2) oxygen type, position of the pt, placement of the BP cuffs, alert status, and pain score to be sent directly to the Electronic Medical Records (EMR) which allows a more detailed overview. In the afternoon, I practised taking manual BP using a sphygmomanometer with my CI. It has been four months since I took manual BP, and I find that there are certain things that I have forgotten, but practising with my CI brings back memories of the steps to perform. It shows me the importance of practising regularly, or I will forget it.
Day 3 (AM)
I tagged with the other CI from morning to lunch. It was a 1:1 session where I learned about bed sponging, applying moisturizers in the most appropriate location, and sharing more about the EMR. Surprisingly, not only when there is a large amount of Bowel Open (BO), 3M Cavilon No Rinse Skin Cleanser can be used as bed sponging without applying any water. I learned that although it is a surgical ward, only ten beds are for surgical cases, and the remaining are considered medical. I was in the MRSA+ cubicle, where I had to follow contact precautions.
After lunch, our ward CI returned us to the Auditorium for the Nurses’ Day 2024 activities.
Day 4 (AM)
After a few days, I managed to see how the SN in charge of the cubicle handed over the report to the next shift, where I took down important information about the pt and tried to access the EMR system where I could view additional pt’s information that is under my care such as the conditions, physical assessment, doctor’s order, and I&O (Intake and Output) chart. I also saw how Dr conduct their rounds with their consultants.
I went to the organisation’s Auditorium at around 1200 to 1300 hours, where there was a Nurses’ Day celebration. The hospital provided and prepared delicious food; there were drinks and ice cream. When the event started, it was so cute; a group of kindergarten children performed and danced. The CN gave a welcoming address, and there was a sharing by the Deputy CEO, who was previously a CN and a surprise by the CEO to appreciate the nurses. There was also a lucky draw with expensive prizes given away, and there were skits as well.
(click to view the assignment)
Day 5 (School Nurses’ Day 2024)
Our school has celebrated Nurses’ Day 2024 in the Auditorium at 1300 hours with performances, an opening speech by our ADoN, an award presentation, a video of our pioneer nurses, sand art animation, skits, and a stand-down dance between students and lecturers. We were encouraged to report at 1230 hours to visit the booth by the three healthcare clusters outside the Auditorium, where there are gifts and information regarding sponsorship, scholarship, and employment after graduation. There are also booths where you can get ice cream and cotton candy. Before and after the event, most students took group photos with their peers or even together with their lecturers.
An important keynote of the event would be this year, which marks the final batch of the Nitec of Nursing and the first batch of Higher Nitec in Nursing. The WSDip (Work-Study Diploma) in Nursing will start on 30 September 2024 in collaboration with industry partners. It is eligible to Nitec in Nursing alumni with a GPA of 2.0 or the new Higher Nitec in Nursing with a Pass, a minimum of one year of working experience and sent by the employer to the course. There have also been changes to the uniform design.

Attendance is compulsory even with a Medical Certificate (MC). A CP replacement will have to be done on Saturday for the entire shift.
Day 8-9 (AM), Day 10 (PM)
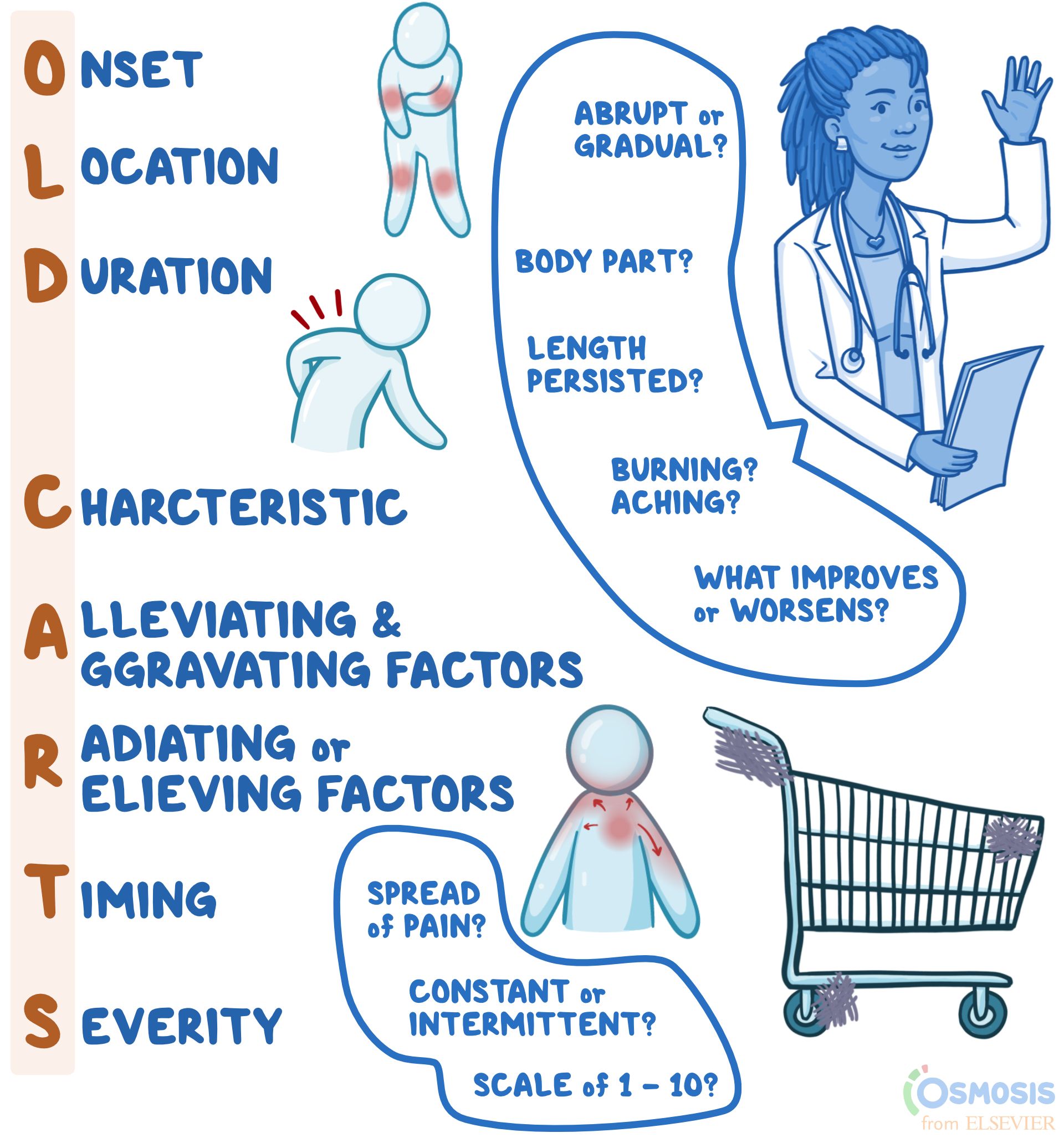
The CIs have worked hard to create activities to help us learn from 1400 to 1600 hours during our second week. On Day 8, we had to know the basics of vital signs; on Day 9, we revised Fulmur’s SPICES bundle care; and on Day 10, we learnt the types of pain assessment tools and scenarios given where we had to act as a pt or nurse and apply OLD CARTS, a history (hx) taking mnemonic.
I am also more familiar with using the EMR, and throughout these few days, I am with different staff during the PM shift as our CI only works during office hours. Most of the staff thought that I was the same age as my peers, and when I revealed my actual age, they were pretty shocked. I met the younger ENs who are in the same school as me.
The NE also brought us to the ward we will be going to next week: A ward with a bus stop theme and a smart ward that gives a hotel backpacker vibe. The smart ward has a bed that shows a different colour of light to indicate whether there is safety, and there is a device where it can automatically calculate the amount of food that the pt eats and automatically upload it to the EMR without manually keying in the I&O chart. How cool isn’t it? I was in the MRSA+ cubicle most of the time, where it was always a reminder to practice good hygiene. I also observed the new admissions, specimen dispatching, and oropharyngeal suctioning procedures.
Day 11 (Last Day, PM)
Our ward CI told us to report to work earlier, at 1230 hours, and once I arrived, my CF said to me that the CIs had ordered food for us.

I brought ice cream and yoghurt as a small gesture to the CIs and ward staff for taking care of us and giving us snacks and drinks during our journey for X2/52.
We chatted during the meal and after eating.
The PM shift students went to the room individually to receive feedback from the CI about their performance during their surgical ward journey.
We then headed to the training centre, where we were given gifts by our ward CI and had to do an evaluation survey for the organisation and from our school.
We spent our final two hours interacting as we did not see each other as frequently as before due to going to the medical ward the following week.

After the interaction section, I returned to the ward at 1600 hours, just five hours before my shift ended. I was attached to an EN, and I applied urosheath to a pt, taking hypocount and feeding a pt who was dangerously ill.
Throughout my journey in the surgical ward, I have been impressed with the EMR, which shows full, comprehensive details with an excellent user interface and user experience. I thought about the previous EMR I used in the vaccination centre and TCF. It turns out that this software is more advanced than the previous one, allowing me to learn more about the patient I am managing. I was fortunate to have one to two students attached to one CI, allowing us more learning opportunities.
Next week, I will be going to the medical ward, my final and most extended posting, before returning to school. I have received the first two weeks of allowance.
Medical
Date: 12 August 2024 – 15 September 2024 (Week 6-10)
Shift: 0800-1600 (AM), 1300-2100 (PM)
Day 1 (Orientation, AM)
The ward I am attached to is higher class, fast medicine, and they also handle a few geriatric cases. I reported at 0750 hours to an ANC, and we have three other CIs who are also ANCs. The deployment is similar to my time in the surgical ward. I followed the handing and taking over, and on my ward, it is more common to see younger patients as I have been handling older patients during my past experiences. It was a routine where I performed vital signs and showered pt in a commode, and during lunch, there was a buffet, and we went. There has been so much celebration in this hospital attachment. Our CF has also reminded us to get our skills signed as the seventh month is coming, which is the Hungry Ghost Festival, where fewer admissions might occur.
Day 2 (PM)
I reported to work and checked the deployment; my assignment was the same cubicle. I was checking my cases, and my CF passed me a case study where I had to find out the condition of the patient, which was to be submitted by Week 3. I also had a chance to talk to one of the experienced nurses assigned from the other ward to help out. The SN of my cubicle is under the Career Conversion Programme (CCP), too, but under a degree, and I have been working for over a year. I have learned a few things from him and assisted him and the other HCA with ADLs. Our CIs went through manual BP again, and we had our competency signed. As usual, it was a fast day, and one of the pt has been DC (discharged).
Day 3 (PM)
Nearer to the end of our shift, our CIs acted in two scenarios, one being a nurse. The other was a pt: the first was taking a postural BP for a patient, and the second was bringing the pt to shower, where we (students) had to highlight what was wrong in the situation, mainly the approach to pt, communication and safety. After which, we students must act on a better version of it.
Day 4 (AM)
As I am attached individually to a CI, and they only work on the AM shift, I performed multiple skills and got it signed. Several times, a nurse, doctor, and pharmacist have asked me to translate from English to Mandarin and Hokkien for the patient. I realised how terrible I was and needed further improvement in my language. So, it is one of my to-do lists before I complete my course, and I also intend to learn Malay and simple Tamil to communicate with my pt better.
Day 5 (PM)
I switched my shift with one of the students as she was having a school CCA, and in return, she had to switch with me the other day. My assignment was in the female cubicle, and there were fewer skills which I could perform. However, I managed to do an NGT feeding, and the concept is similar to NH’s. The NE passed by and provided tips on how I can provide better care for the pt. I have also assisted the physiotherapist (PT) in performing a distance walk test using a rollator frame for a patient, a skill I haven’t done for over a year. During the afternoon, there was not much movement, so I looked through the organisation’s intranet to use my time to review their documents, Standard Operating Procedures (SOP), and case notes of the pt to understand the condition better. During my break time, there was a computer in the room, and I took the opportunity to look at a case note for a pt who has been DC to improve my case study further.
Week 2-4
As usual, our CI trainees will be changed every two weeks, and there will always be activities organised, a food celebration and gifts given to us. During our last week (week 5), there will only be a CI from the ward, which is the norm. The good news is that the newer batch of students will have CI trainees again. This is due to the hospital’s future expansion and training of newcomers. Since coming to the hospital, I noticed quite a few staff members under probation and were attached to a preceptor. An EN that I interacted with was going for the WSDip in Nursing programme in September 2024. As a local, let’s be thankful for what we have instead of being demanding. I learned that those not local are typically bonded for six years after completing their Diploma in Nursing.
Our NE always reminded us about the perspective, the story of one big and small watermelon, but they are the same, and it depends on how you think. An example would be, instead of saying, “There are three more weeks of internship”, think “, I have already completed seven weeks of my internship; what can I do to improve myself further in the next three weeks?” Before joining the hospital, I had heard many stories that the hospital was too fast-paced and stressful. Still, after I had experienced it myself, I believe it depends on the organisation and the ward you are in. Aside from my school and throughout the weeks. The staff and patients were generally lovely, and I had no negative encounters. I found that the working pace was slower than while I was working in a TCF as they have reduced the manpower by almost half after joining them for a week. As I recall, there was a night shift where there was only me and another HCA, and we had to manage nine regular patients and three isolated patients (two MRSA+ and one scabies). What I find about hospitals is that they emphasise SOPs and documentation compared to step-down care like your NH.
Week 5 (Last Week)
I am familiar with the routine and can do most things independently.
| Time | Routine |
|---|---|
| 0800 – 0830 | AM Huddles and HOTO (Handing Over and Taking Over) |
| 0815 | Charting down I&O for Breakfast |
| 0815 – 0945 | Showering, Bed Bath, Tepid Sponging |
| 0945 – 1000 | Q4H (4 Hourly) Para (Vital Signs) |
| 1115 – 1130 | Lunch POCT (Blood Glucose Monitoring) |
| 1130 – 1200 | Assisting with Lunch and charting down I&O |
| 1300 – 1330 | PM Huddles and HOTO |
| 1345 – 1400 | Q4H / TDS (Three Times A Day) Para |
| 1715 – 1730 | Dinner POCT |
| 1730 – 1800 | Assisting with Dinner and charting down I&O |
| 1745 – 1800 | Postural BP BD (Twice a Day) |
| 2000 – 2030 | Night Huddles and HOTO |
During week 4, I was informed by my CI that I received a compliment from a patient who has been DC. Upon hearing the news, I was pretty touched. I felt I hadn’t done my best, and something unexpected happened this week. Another pt who has been DC, I received the following message on social media from his son:
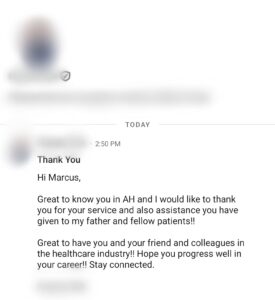
It is a memorable experience I will never forget. To this day, I still appreciate that I was allowed to be in nursing, and I thank the HCWs and patients for guiding me in my journey.
I managed to complete 28 skills out of the 36 skills. I would say most skills are available, and you should have nothing to be worried about. My ward has a mixture of alternate male and female patients. So, if you are a male, you will have fewer opportunities than your female schoolmates, as there are specific procedures you can’t perform on a female pt. Constantly learn and know the rationale of why you are doing the skill. Don’t do things to get the logbook signed and just for the certificate.
I have seen how the hospital operates, and the school does things. This allows me to plan my future and make better decisions.
A bonus: I have asked for opinions on whether Diploma in Nursing at NP (Ngee Ann Polytechnic) or NYP (Nanyang Polytechnic). The answer was that if you are more of a practical person, go for NYP, while if you prefer SDL (Self Directed Learning), go for NP.
Thank you for reading this lengthy post. It is my first experience. I am on my two-week term break before returning to school, and the next CP (CP2) will be in six months, including a one-week special posting in IMH (Institute of Mental Health) and Polyclinic settings. I can’t wait! Until then, I will try to post regularly and see you soon.